Science Meets Compassion in Every Treatment
Choose a treatment to explore your options.

IUI (Intrauterine Insemination)
Intrauterine Insemination (IUI) is a commonly used fertility treatment that involves placing specially washed and concentrated sperm directly into a woman’s uterus around the time of ovulation. This procedure increases the chances of fertilization by bringing the sperm closer to the egg.
Who is IUI for?
- Couples with unexplained infertility
- Mild male factor infertility (such as low sperm count or motility)
- Women with cervical mucus problems
- Individuals using donor sperm
- Couples facing sexual dysfunction or ejaculation issues
Procedure Steps
- Ovulation Monitoring: Hormonal medications may be used to stimulate ovulation, and ultrasound scans track the follicle development.
- Semen Preparation: The partner’s or donor’s sperm is collected and processed in a lab to isolate the healthiest sperm.
- Insemination: The prepared sperm is inserted directly into the uterus using a thin catheter. This is a quick and generally painless procedure.
- Post-Insemination: Patients rest briefly and resume normal activities. A pregnancy test is done after 2 weeks.
Benefits of IUI
- Non-invasive and relatively painless
- More affordable than IVF
- Suitable for various mild fertility issues
- Can be repeated over multiple cycles if needed
Success Rates
Success rates vary depending on age, underlying cause of infertility, and whether fertility medications are used. Typically, success rates range from 10% to 20% per cycle.
Risks & Considerations
- Minimal risks, such as mild cramping or spotting
- Slight chance of multiple pregnancy if ovulation is stimulated
- Emotional stress due to waiting and uncertainty
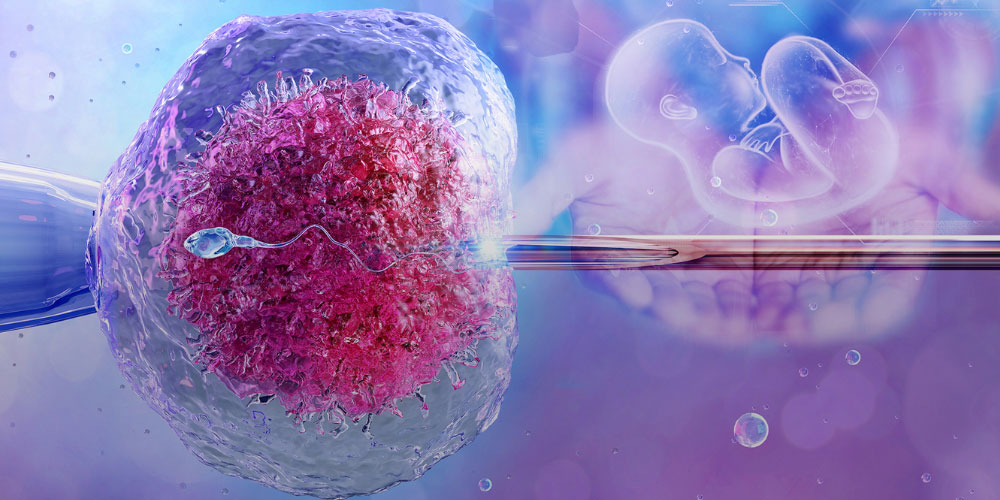
IVF(In Vitro Fertilization)
In Vitro Fertilization (IVF)is a complex series of procedures used to help with fertility or prevent genetic problems. It involves combining an egg and sperm outside the body in a laboratory and then transferring the embryo into the uterus.
Who is IVF For?
- Women with blocked or damaged fallopian tubes
- Couples with unexplained infertility
- Women with ovulation disorders
- Men with low sperm count or motility
- Women with endometriosis
- Individuals or couples using donor eggs or sperm
- Couples with genetic disorders they wish to avoid passing on
- People who failed other fertility treatments like IUI
IVF Procedure Steps
- Ovarian Stimulation: Hormonal injections are given to stimulate the ovaries to produce multiple eggs.
- Monitoring & Egg Retrieval: Follicle development is tracked via ultrasound. Eggs are retrieved under mild anesthesia using a needle guided by ultrasound.
- Sperm Collection & Fertilization: A sperm sample is collected and the healthiest sperm are used to fertilize the eggs in the lab (via traditional IVF or ICSI).
- Embryo Culture: The fertilized eggs are monitored for a few days as they develop into embryos.
- Embryo Transfer: One or more healthy embryos are transferred into the uterus using a thin catheter. This is a painless procedure.
- Post-Procedure & Pregnancy Test: A pregnancy test is taken about 10–14 days after embryo transfer to confirm success.
Benefits of IVF
- High success rate, especially with advanced lab techniques
- Helps with multiple infertility causes (male, female, or unexplained)
- Can use donor eggs, sperm, or embryos
- Genetic testing of embryos is possible (PGT)
- Gives same-sex couples or single individuals a chance to conceive
Success Rates
IVF success varies depending on:
- Age of the woman
- Egg and sperm quality
- Cause of infertility
- Number of previous IVF attempts
Generally:
- Women under 35: 40–50% success per cycle
- Ages 35–40: 30–40%
- Over 40: 10–20%

ICSI (Intracytoplasmic Sperm Injection)
ICSI is an advanced fertility treatment used in conjunction with IVF. In this procedure, a single healthy sperm is directly injected into an egg to facilitate fertilization. It is especially beneficial for cases involving severe male infertility or previously failed fertilization.
Who is ICSI for?
- Men with very low sperm count or motility
- Cases of abnormal sperm shape or function
- Men who have had a vasectomy or other reproductive tract blockages
- Couples who had poor or failed fertilization with standard IVF
- Use of previously frozen sperm or eggs
- When sperm is retrieved surgically (e.g., from testes or epididymis)
ICSI Procedure Steps
- Ovarian Stimulation: Hormonal medications are given to the woman to stimulate the ovaries and produce multiple eggs.
- Egg Retrieval: Eggs are collected from the ovaries using ultrasound-guided aspiration under sedation.
- Sperm Collection & Selection: A semen sample is obtained (or retrieved surgically), and the healthiest sperm is chosen under a microscope.
- Sperm Injection (ICSI Step): A single sperm is carefully injected into the center of each mature egg using a fine glass needle.
- Fertilization & Embryo Development: Fertilized eggs are monitored in the lab for several days to allow embryo development.
- Embryo Transfer: One or more healthy embryos are transferred into the woman’s uterus to establish pregnancy.
- Pregnancy Test: A blood test is done after about 2 weeks to confirm pregnancy.
Benefits of ICSI
- Overcomes severe male infertility issues
- Enables fertilization even with very few or poor-quality sperm
- Ideal when fertilization failed in prior IVF cycles
- Helps when using frozen sperm or surgically retrieved sperm
- Boosts chances in cases of unexplained infertility
Success Rates
Success depends on factors such as age, egg and sperm quality, and clinic expertise. ICSI success rates are generally comparable to or slightly higher than standard IVF, with fertilization success rates over 70–80%. However, the live birth rate per cycle ranges from 25% to 45%, depending on the patient profile.
Risks & Considerations
- Slightly higher cost compared to conventional IVF
- Risk of fertilization failure in rare cases
- Minimal risk of damage to eggs during injection
- Emotional stress associated with treatment outcome
- Slight increased risk of genetic abnormalities (especially when male infertility is genetic)

Fertility Preservation
Preserving your fertility can help you plan for the future — whether due to medical reasons or personal choice. Fertility preservation involves protecting eggs, sperm, or reproductive tissues to be used at a later time.
Who is Fertility Preservation for?
- Individuals undergoing cancer treatment (chemotherapy or radiation)
- People with medical conditions affecting fertility
- Women who want to delay childbearing for personal or career reasons
- Couples planning to postpone pregnancy but want to preserve their reproductive cells
Preservation Options:
- Egg Freezing (Oocyte Cryopreservation): Mature eggs are retrieved, frozen, and stored for future use.
- Embryo Freezing: Fertilized embryos are created and frozen for later transfer.
- Sperm Freezing: A quick and effective method for preserving male fertility.
- Ovarian Tissue Freezing: An experimental option involving the freezing of ovarian tissue.
Procedure Overview:
- Medical evaluation and fertility assessment
- Use of hormonal medications to stimulate egg production (in egg/embryo freezing)
- Egg retrieval under ultrasound guidance
- Freezing and secure storage of eggs, embryos, or sperm in a cryogenic facility
Benefits of Fertility Preservation:
- Offers hope for future biological parenthood
- Protects fertility before medical treatments or aging impacts reproductive health
- Allows individuals and couples to plan parenthood on their own timeline
Considerations & Risks:
- No guarantee of pregnancy later
- Costs may vary and are not always covered by insurance
- Success depends on age and method used
Ovarian Stimulation & Monitoring
Ovarian stimulation is a critical step in assisted reproductive treatments such as IUI (Intrauterine Insemination) and IVF (In Vitro Fertilization). Its main goal is to encourage the ovaries to produce multiple eggs, increasing the chances of successful fertilization and pregnancy.
Why Stimulate the Ovaries?
In a natural menstrual cycle, a woman typically releases one egg per month. However, for fertility treatments, more eggs are needed to improve success rates. Fertility medications, such as Clomiphene Citrate, Letrozole, or gonadotropins, are prescribed to gently stimulate the ovaries to produce multiple mature follicles.
How is the Process Monitored?
Ovarian stimulation must be closely monitored to ensure safety and effectiveness. The key steps include:
-
Baseline Scan & Blood Tests:
- Conducted before starting medications to check the uterus and ovaries.
- Hormone levels like FSH, LH, and Estradiol are assessed.
-
Ultrasound Monitoring:
- Transvaginal ultrasounds are performed regularly (every 2–3 days).
- They track follicle size and number in the ovaries.
-
Hormone Level Monitoring:
- Blood tests measure estradiol (E2) levels.
- Helps determine follicle maturity and prevent overstimulation.
-
Trigger Shot:
- When follicles reach the desired size (18–20 mm), an hCG injection is given to mature the eggs for ovulation or retrieval.
Personalized and Safe Approach
Every woman’s body responds differently to stimulation. Monitoring ensures that medication doses are adjusted as needed and that the risk of complications such as Ovarian Hyperstimulation Syndrome (OHSS) is minimized.
Outcome
- In IVF, egg retrieval is scheduled 34–36 hours after the trigger shot.
- In IUI, insemination is timed precisely after ovulation.
- Multiple mature eggs improve the chance of fertilization and embryo development.
Summary
- Improves fertility treatment outcomes
- Prevents complications
- Allows individualized treatment protocols
With the right balance of medication and expert monitoring, this phase significantly enhances the success of fertility treatments.
Ovulation Induction
Ovulation Induction is a fertility treatment that involves stimulating a woman’s ovaries to produce and release one or more eggs in a controlled manner. It is primarily used for women who have irregular or absent ovulation (anovulation).
How It Works
- Fertility medications such as Clomiphene Citrate or Letrozole are prescribed to stimulate ovulation.
- Hormone levels and follicular development are closely monitored through blood tests and ultrasound scans.
- Once a mature follicle is detected, a trigger injection (usually hCG) is administered to induce ovulation.
- Timed intercourse or Intrauterine Insemination (IUI) may be recommended around the ovulation window.
Who Can Benefit?
- Women with Polycystic Ovary Syndrome (PCOS)
- Women with irregular or absent periods
- Those trying to conceive for a prolonged period without success
Benefits
- Simple and non-invasive treatment
- Relatively low cost compared to advanced fertility treatments
- Can be combined with other treatments like IUI
Risks
- Multiple pregnancy (twins or more)
- Ovarian Hyperstimulation Syndrome (rare)
- Mood swings or abdominal discomfort
Ovulation induction is often the first step in treating infertility and helps many couples achieve a successful pregnancy with minimal intervention.

Donor Programs
Donor Programs help individuals or couples conceive using donated eggs, sperm, or embryos when using their own is not possible or advisable.
Types of Donor Programs:
- Egg Donation: Eggs from a donor are fertilized and transferred to the recipient’s uterus.
- Sperm Donation: Donated sperm is used for IUI or IVF.
- Embryo Donation: Donated embryos from other couples are used for implantation.
Who Can Benefit?
- Women with premature ovarian failure
- Men with no sperm production
- Couples with genetic concerns
- Single women or same-sex female couples
- Those with multiple IVF failures
Note: All donors are thoroughly screened, and programs follow ethical and legal guidelines strictly.

Surrogacy
Surrogacy is an arrangement where a woman (the surrogate) carries and delivers a baby for a couple or individual who is unable to conceive or carry a pregnancy themselves. It is a method of assisted reproduction used when medical or personal reasons prevent intended parents from having a biological child.
Types of Surrogacy
- Gestational Surrogacy: The surrogate carries a baby conceived through IVF using the egg and sperm of the intended parents or donors. The surrogate has no genetic link to the baby.
- Traditional Surrogacy: The surrogate's own egg is used, making her the biological mother. This method is less common due to legal and emotional complexities.
Who Can Benefit from Surrogacy?
- Women with medical conditions that prevent pregnancy (e.g., absence of uterus, recurrent miscarriage).
- Couples who have failed multiple IVF attempts.
- Individuals or couples with genetic concerns.
- Same-sex male couples or single men wishing to have a biological child.
Steps Involved in Surrogacy
- Screening and Legal Agreements: Thorough medical and psychological screening is done for both the surrogate and intended parents. Legal agreements are signed to protect all parties involved.
- IVF and Embryo Transfer: Embryos are created in the lab using IVF and then transferred into the surrogate’s uterus.
- Pregnancy and Monitoring: The surrogate undergoes regular prenatal care and monitoring throughout the pregnancy.
- Delivery and Legal Custody: After birth, legal procedures ensure the baby is handed over to the intended parents, and custody is transferred according to pre-signed agreements.
Benefits of Surrogacy
- Enables parenthood for individuals or couples who cannot conceive.
- Offers a biological connection in the case of gestational surrogacy.
- Legally secure with proper agreements in place.
Considerations
- Emotional, legal, and financial aspects must be clearly discussed.
- Choosing a reputable clinic and legal advisor is crucial.
- Surrogacy laws vary from country to country — always ensure legal compliance.
